“The new normal.” We’ve all been hearing that phrase since the beginning of the pandemic and can’t wait until everything is indeed, “back to normal”. But the reality is COVID-19 has changed so much of our daily lives and the way we practice healthcare is included. Here are some ways healthcare will look different in the post-pandemic world.
Increased Use of Pharmacies
Pharmacies continue to play a vital role in the triumph of COVID-19. Pharmacists were and still are, the easiest clinician to access throughout the pandemic and were handling numerous tasks such as answering patient questions about the virus, distributing medications, testing, and now administering vaccines. Pharmacies went to extraordinary lengths to make sure they were delivering the safest and most effective care to their patients, by limiting the number of people inside at once, temperature checking staff and patients daily, creating drive-throughs and curbside pickups, expanding home delivery services, dispensing 90-day fills to avoid additional trips to the pharmacy, conducting virtual visits with patients, and much more.1
According to this year’s annual Gallop Poll, pharmacists ranked fourth in the most trusted profession, behind nurses, doctors, and school teachers, with 71% of respondents having a very high/high confidence in pharmacists. Their rating increased seven percentage points from 2019, which was the second-highest raise behind doctors, who went up to twelve percentage points from last year. It is clear that patients love utilizing their pharmacist’s knowledge and expertise, and we should expect to see their role in care drastically increase over time.
Preventative Healthcare
You probably know someone (or multiple people) who has not been to the doctor in years, and whatever ailment/injury they suffer will just “go away” or can be cured by “rubbing some dirt on it.” Hopefully, COVID-19 will change that mindset, encourage people to schedule regular check-ups, and be proactive with their health. In fact, early reports are showing that it already has.
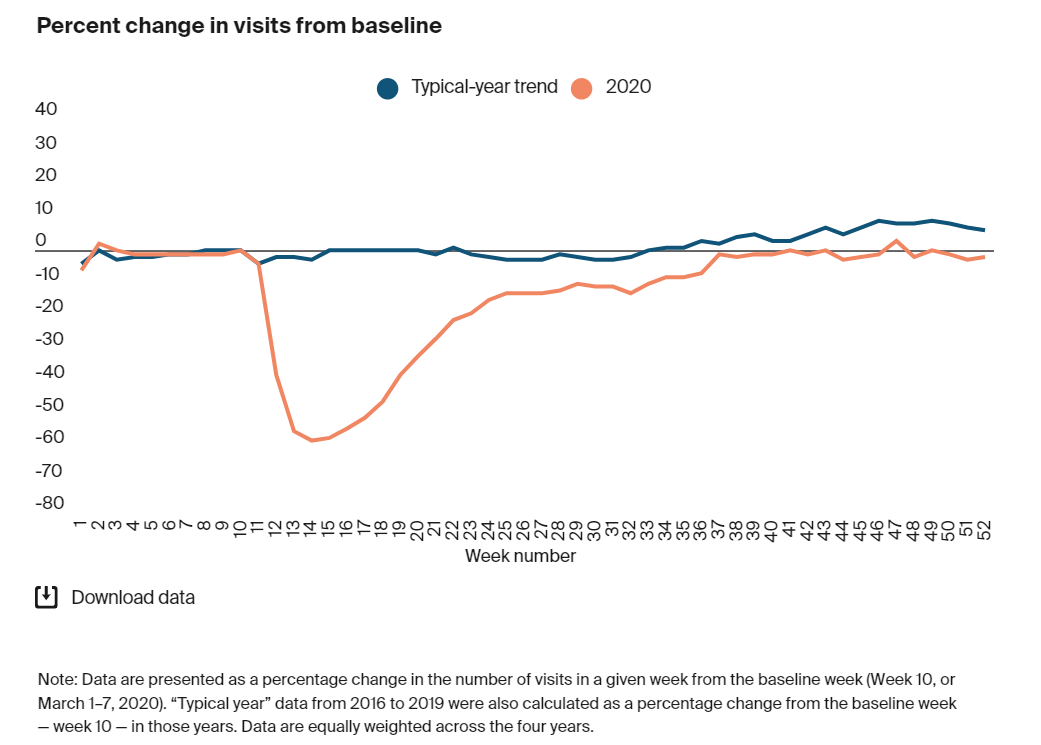
As you can see in this chart above, during April of 2020, outpatient visits dropped nearly 60% compared to a typical year. Now, the numbers are back up to or near pre-pandemic rates, and have even shown improvement in some specialties, such as rheumatology, urology, endocrinology, oncology, and adult primary care.2 Regarding COVID-19, with the right insurance, testing is free! Even if your only symptom is a little cough, it cannot hurt to get tested.
Cost
When countries began going into lockdown, healthcare revenue took a big hit. Hospitals had to shut-down non-emergency procedures, and patients were cancelling their routine appointments with their primary-care physicians. Now, with vaccines rates increasing and new case-rate decreasing, patients will resume with their elective procedures and regularly scheduled check-ups. However, when surgeries are delayed and appointments cancelled, the severity of the condition, or whatever issue a patient developed in the past year, will be harder and more expensive to treat. For example, women who cancelled mammograms or pap smears may have developed breast or cervical cancer, which would have been easier and cheaper to treat if they had found it a year earlier.
Along with the cost of treatment, we may see an increase in drug prices as well. In fact, the Vizient Winter 2021 Pharmacy Market Outlook projected a 2.67% increase in the price of pharmaceuticals purchased by health organizations within the next twelve months. This was caused by financial difficulties created by the pandemic.3
Patient-Centered Care
The good news is many organizations are allocating some of their revenue towards new patient-centered initiatives. Patient-centered care is when the provider designs treatment around a specific individual, as opposed to a group or specific disease or illness. Because healthcare is not a “one size fits all” tactic, providers must go the extra mile and address all social determinants of health if they want what’s best for their patients.
Empowering the patient is the focus of this approach, and one way providers can achieve this is by shared decision making. By collaborating on treatment plans, trust is established between patient and doctor, and studies show that the greater the relationship between the two parties, the greater the outcomes.4 Some other empowerment strategies providers implemented during the pandemic included online appointment scheduling, access to patient portals and health information, virtual visits, and other means of delivering care from a distance. Technology plays a huge role in patient-centered care.
Telemedicine and Other Technology
Technology in healthcare isn’t a new idea; organizations have been implementing digital health even before the HITECH Act was passed in 2009. However, the pandemic showed just how important technology can be in delivering care.
Telemedicine was the most popular form of health tech throughout the pandemic, with 61% of patients having cited its use at least once. Of that percentage group, 88% said they would like to continue its use even after the virus has passed.5 Before COVID-19 came about, only about 18% of providers offered virtual visits, now that number has climbed to 64%.6 Not only is telehealth more convenient and cost-effective for patients, but it also allowed providers to continue their practice during lockdown and expand their customer reach in process. Telemedicine will continue to play a large role in healthcare.
Other forms of technology include remote monitoring, wearable devices, mobile apps, contact tracing, and more. These allowed providers to connect with patients and monitor their health while remaining socially distant. Wearables and mobile apps can motivate patients to stay fit, by setting step goals, tracking calories, water intake, etc., while contact tracing helped monitor where the COVID-19 hotspots were in and around a specific area. Time will tell what other technologies become mainstream in the industry.
The pandemic put many hardships on hospitals and private practices, forcing them to re-evaluate how they delivered care to their patients. In this “adapt or die” world only the strong survive, and organizations that could not adjust may have closed their doors permanently. Even long after COVID-19 is a threat, it has set a precedent of how the “new normal” will look in the future, and potentially forever.
…………………………………………………………………………………………………………………………………
REFERENCES:
- “Guidelines for Pharmacists in Community Pharmacy.” PharmacistMomsGroup, 17 Mar. 2020, pharmacistmomsgroup.com/guidelines-for-pharmacists-in-community-pharmacy/.
- Mehrotra, Ateev, et al. “The Impact of COVID-19 on Outpatient Visits in 2020: Visits Remained Stable, Despite a Late Surge in Cases.” Impact COVID-19 Outpatient Visits 2020: Visits Remained Stable | Commonwealth Fund, 22 Feb. 2021, commonwealthfund.org/publications/2021/feb/impact-covid-19-outpatient-visits-2020-visits-stable-despite-late-surge.
- Rosenfeld, Samara. “COVID-19 May Continue to Impact Healthcare Costs.” Managed Healthcare Executive, Managed Healthcare Executive, 1 Feb. 2021, managedhealthcareexecutive.com/view/covid-19-continues-impact-healthcare.
- Birkhäuer, Johanna, et al. “Trust in the Health Care Professional and Health Outcome: A Meta-Analysis.” PloS One, Public Library of Science, 7 Feb. 2017, ncbi.nlm.nih.gov/pmc/articles/PMC5295692/.
- Lagasse, Jeff. “Most Consumers Want to Keep Telehealth after the COVID-19 Pandemic.” Healthcare Finance News, 12 Apr. 2021, healthcarefinancenews.com/news/most-consumers-want-keep-telehealth-after-covid-19-pandemic.
- Wyatt, Koma, et al. “Medicare and Telehealth: Coverage and Use During the COVID-19 Pandemic and Options for the Future.” KFF, 19 May 2021, kff.org/medicare/issue-brief/medicare-and-telehealth-coverage-and-use-during-the-covid-19-pandemic-and-options-for-the-future/.
