A clean, successful Revenue Cycle Management (RCM) process is critical to your organization’s fiscal health, and opens the door to providing high quality services and a sustainable work environment. Healthcare revenue cycle is tightly woven into the patient journey, from scheduling the appointment to a zero balance on their account. A solid RCM process ensures timely revenue, steady collections and financial viability, allowing organizations to direct more of their focus on care delivery. Cantata’s RCM solution can help organizations achieve this!
Before we go into what qualities make a good revenue cycle, let’s first review the current issues your staff deal with daily.
High A/R
When the revenue cycle is mismanaged, collection efficiency drops and Accounts Receivable (A/R) days increase. An increase in A/R days means the organization is taking longer to collect payments from patients and insurance companies, which can cause negatives consequences, such as:
- Slower growth of the health system’s business due to diminished cash flow
- Difficulty paying bills on time, which can lead to late fees and penalties
- Trouble recruiting and retaining staff due to uncertainty about the organization’s financial stability
- Harmful impact on the organization’s reputation
Outdated Claims
Outdated and incorrect claims can lead to denials, which will impact the organization’s bottom line. In fact, the denial of a single claim can amount to as much as $100 or more. Unfortunately, denial rates in the US are higher than ever. According to the Change Healthcare 2020 Denials Index, 11.1% of claims were denied upon initial submission between 2016 and the third quarter of 2020.
Human Error
Human error is too often the root cause of many revenue cycle disruptions. For example, if a billing specialist enters the wrong code for a procedure, the insurance company may not pay for it, resulting in lost revenue for the organization and increased costs for the patient. In addition, incorrect information can lead to customer service issues and complaints, damaging the organization’s reputation and bottom line.
Insurance Denials
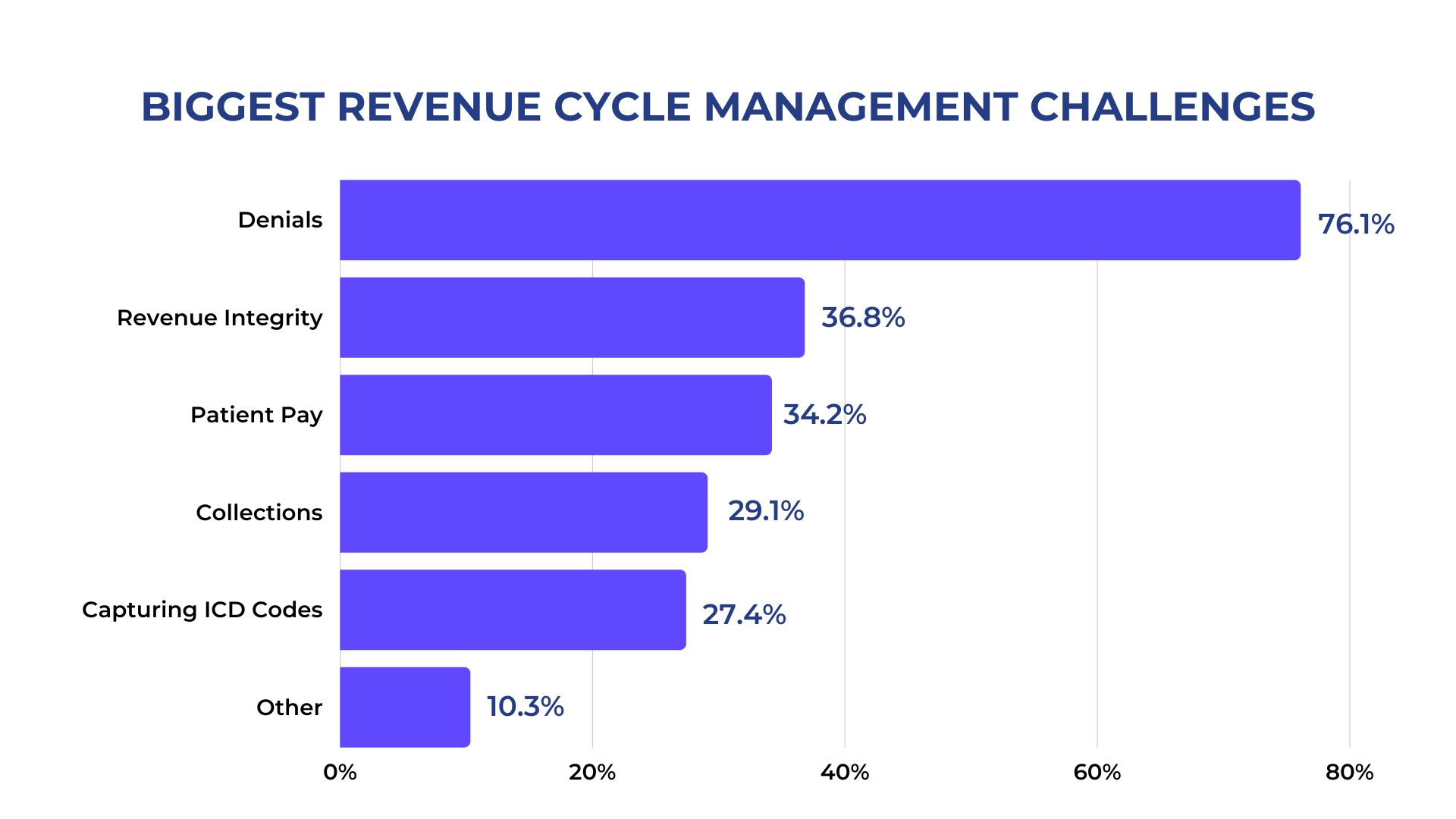
According to a Dimensional Insight survey, 76% of healthcare leaders say denials constitute the greatest challenge they face. When an insurance company denies a payment, it can create a backlog of unpaid claims that can impact the organization’s cash flow, leading to financial difficulties. Denials can also have a negative effect on the client, who may have to pay out-of-pocket for services they thought would be covered by their insurance plan.
How Cantata Health’s RCM Solution can help
Strategy
Claim denials can be aggravating, but about 90% are preventable. Developing a strategy is the first step toward reducing their frequency. Having a set of specific, step-by-step procedures in place for how your staff handle billing and claims will make the process more consistent, and less likely to result in errors. We have a team of highly experienced, senior-level healthcare IT executives with deep a understanding of the specific requirements of healthcare billing who will work with your team to develop those current best-practice procedures. Our staff provides the expertise to help you build and execute the strategic plans and initiatives that will help you work toward eliminating denials.
Understand reasoning for rejection
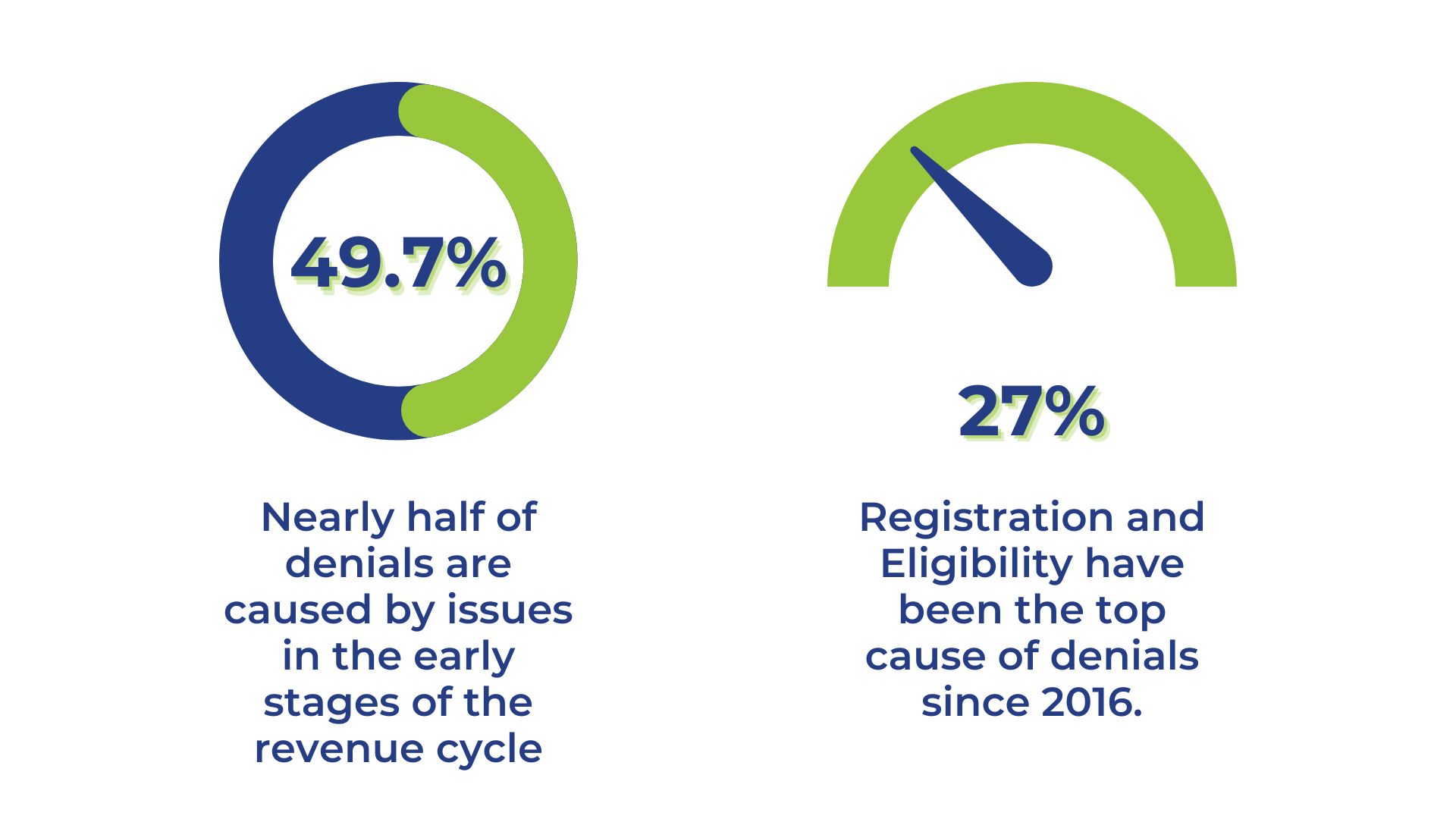
It is important to understand why your claim was rejected in the first place. Reasons for rejection can vary, but common causes include incorrect information on the claim form, missing documentation, or a discrepancy between the billing code and the service provided. Analysis from the Change Healthcare 2020 Revenue Cycle Denials Index showed approximately half of denials are caused by issues in the early stages of the revenue cycle. Cantata’s Black-Book recognized Revenue Cycle Management solution, provides users the ability to identify those early mistakes by giving administrative staff full visibility into every detail of the claim.
Tracking/Analyzing Trends
Analyzing revenue cycle trends helps identify and correct potential problems before they cause major disruptions to your cash flow, and they can be tracked through financial reports, insurance data, and patient surveys. For example, if it is found that many patients are being charged incorrectly for services, then steps can be taken to correct the billing process. Alternatively, if it is found that many patients are not paying their bills, then steps can be taken to improve collections efforts. Cantata Health Solutions gives providers the analytical foresight to improve successful billing rates at their organization. Our predictive analytics tools help your staff identify and categorize denials into high, mid-range, and low values, accelerating resolutions in all three categories.
Pre-collection of forms
Most health systems are inundated with paperwork, including insurance verification, authorization, and intake forms. The more efficiently you manage this paperwork, the less time you will need to spend on administrative tasks. Organizations should provide patients the required forms ahead of each visit and encourage them to complete the forms beforehand – it’s a win-win scenario for both parties. Having patients complete their own documentation saves time and effort for provider administrative staff, and decreases time spent in the waiting room for patients.
This can also increase accuracy, as patients may have an easier time filling out their contact and insurance information at home, without the distractions and stress they may experience in the waiting room. Cantata Health’s Family and Consumer Portal allows patients to complete their documentation at home before their visit, as well as schedule future appointments, pay bills, message providers, access their health records, and more!
Experienced Staff
Cantata is a top provider of healthcare solutions across a variety of settings, including behavioral health, human services, acute, and post-acute care. We have been supporting clients with our industry-leading RCM solution since 1977. Collectively our staff has over 250 years of experience in the healthcare market, developing, implementing, and maintaining effective healthcare IT solutions.
Short- and Long-Term Benefits
Revenue cycle management solutions are essential to ensure your organization gets paid for the services it provides. As we move toward value-based reimbursement, RCM helps your organization remain financially healthy so you can stay focused on providing superior care. Such benefits include:
- Reduced errors
Organizations must ensure their revenue cycle is as streamlined as possible to avoid mistakes and bill patients accurately and on time. An RCM solution can help reduce errors by automating many of the tasks involved in the billing process. Additionally, an effective solution provides staff with detailed reports on charges, helping them quickly identify and correct issues.
- Lower costs
Billing errors can create unnecessary and costly expenses for organizations. An efficient RCM solution will help staff better manage receivables, creating a more accurate picture of your financial position. This allows healthcare leaders to make more informed decisions about how to allocate resources.
- Fewer denials
Claim denials can be detrimental to your organization and create headaches for your team. Although they’re quite common in healthcare, there are plenty of ways to manage them. Having an effective RCM solution allows your staff to be proactive, and gives them the power to stay on top of client information and insurance policies, ensuring all the information is accurate and up to date. This will help decrease the number of denials and improve your reimbursement rates.
- Faster collection process
Another benefit is that it can help speed up the collection process. By automating many of the tasks involved, an RCM solution can bill patients more quickly and get organizations paid sooner. This is especially helpful when dealing with a large volume of invoices. Getting payments processed faster will improve cash flow.
- Reduced administrative burden
Burnout is one of the major issues in the workforce today, and one of the most impacted industries is healthcare. While we often associate burnout with doctors and nurses, administrative staff feel a heavy burden as well. An RCM solution can cut a lot of the tedious work administrators deal with on a daily basis. Automating tasks such as registration, billing, and insurance verification can save a tremendous amount of time that staff could spend attending to other important issues or responsibilities.
- Improved patient experience
With consumerism taking over healthcare, improving client satisfaction should be a top initiative for organizations. Patients of today are seeking a seamless experience from the moment they schedule an appointment to the moment they receive their bill. RCM solutions can help reduce the amount of time patients have to wait for their bills to be processed, eliminating the stress and frustration associated with it. This allows patients to focus on their treatment, and not on payment concerns. By giving clients online access to their fees, they can easily track the process and better manage their finances. This improves communication and overall satisfaction.
If your organization doesn’t have a revenue cycle management solution in place, you’re putting your financial health at risk. Without one, you could find yourself struggling to pay bills, which could put the future of your organization in jeopardy. Investing in a quality solution like Cantata’s RCM can improve your bottom line, staff productivity, patient experience, and thus your reputation. Our RCM solution helps your staff better understand your clients, reasons for denials, and financial trends, reducing errors, lowering costs, and improving profits. Cantata understands that a clean revenue cycle is directly linked to fiscal health, and we are committed to providing solutions that will help your organization achieve its goals.
