Close
This article was originally published on Behavioral Health News by Dr. Jorge R. Petit, Chief Clinical Advisor
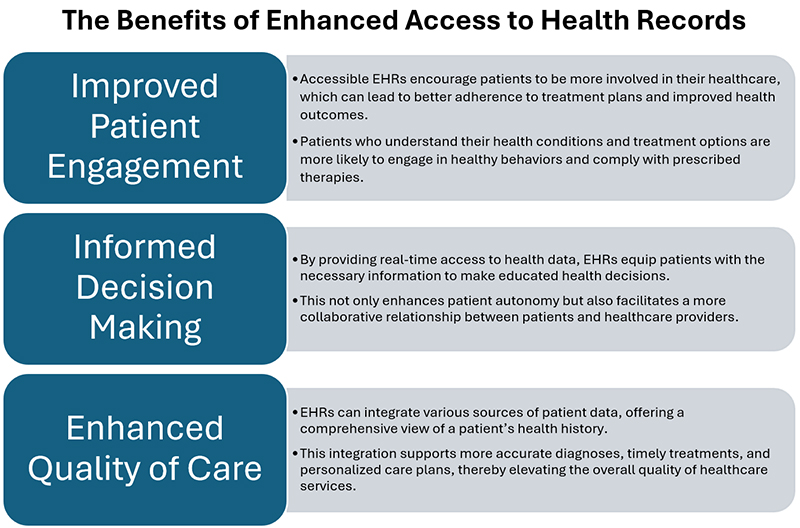
The integration of digital technology in healthcare has ushered in a new era of patient empowerment, providing an unprecedented level of engagement and autonomy in managing one’s health by enabling easier access to electronic health records (EHRs). This transformation has significantly altered the dynamics of patient-provider interactions, allowing patients greater control (empowerment) and enhancing their involvement in shared decision-making (engagement), their engagement, and shared decision-making in their healthcare process.
The trend in developing more accessible EHRs is a cornerstone of contemporary healthcare reform initiatives, reflecting a broader transition towards a more digital, data-driven healthcare environment. This movement has profound implications for all stakeholders in the healthcare ecosystem—from patients to policymakers and technology developers—and, most critically, the behavioral healthcare (BH) sector.
Historically, the BH sector has received less financial support compared to general medical care when it comes to adopting health information technology. For instance, while the Health Information Technology for Economic and Clinical Health (HITECH) Act of 2009 provided substantial funding for hospitals and clinics to implement EHRs, behavioral health providers were largely excluded from these federal incentives, resulting in a slower adoption rate of EHRs in behavioral health practices, especially in smaller clinics and community mental health settings, which often operate with limited resources.
Behavioral health services in the U.S. are often provided by a patchwork of public and private entities, including community health centers, private practices, non-profit organizations, and state-run facilities. These systems tend to be underfunded and lack the financial capital to invest in advanced technological infrastructure, making it difficult to implement electronic health records that are interoperable within the broader healthcare ecosystem. The result is siloed systems of care that are unable to fully participate in the technological advancements seen in general healthcare.
To further complicate matters, BH data, such as psychiatric evaluations, therapy notes, and substance use treatment plans, contain more sensitive information than physical health data. This makes it more challenging to integrate behavioral health data into standardized electronic health records that are designed primarily for physical health. There are also additional privacy concerns with mental health and substance use disorder data, leading to more stringent confidentiality regulations (e.g., 42 CFR Part 2) compared to general healthcare, making data sharing and system integration more challenging.
All too often, behavioral health EHRs have been developed as standalone systems, making it difficult for behavioral health providers to share data with other healthcare providers in an integrated fashion. As a result, critical information about a patient’s mental health, substance use, and overall treatment plan may not be readily available to primary care providers or specialists, leading to fragmented care and poorer outcomes. This lack of interoperability exacerbates the gap between behavioral health and general medical care, limiting the potential for coordinated, whole-person care.
The slower adoption of technology in BH has profound consequences for the quality and accessibility of care. Patients with mental health and substance use disorders often require integrated, coordinated care across multiple providers. Without interoperable electronic health records, behavioral health providers face challenges in accessing and sharing critical information, and patient outcomes are impacted.
The move towards more accessible EHRs is not merely a technological upgrade but a profound shift towards a more inclusive, efficient, and patient-centered healthcare system. This transition is pivotal for the future of behavioral healthcare delivery, promising significant improvements in patient outcomes, system efficiency, and public health management.
The move towards more accessible EHRs is not merely a technological upgrade but a profound shift towards a more inclusive, efficient, and patient-centered healthcare system. This transition is pivotal for the future of behavioral healthcare delivery, promising significant improvements in patient outcomes, system efficiency, and public health management.
While the benefits are clear, there are three significant challenges that need to be addressed when implementing such technologies:
1. Data Privacy and Security
Ensuring the data privacy, confidentiality, and integrity of health data is paramount, especially in BH. The expansion of EHR accessibility brings substantial benefits but also introduces significant risks that must be carefully managed to protect sensitive patient information. Patient confidentiality is a core principle of healthcare, with more confidentiality restrictions for BH data, and EHRs must ensure that sensitive health information is only accessible to authorized individuals. As electronic health records become more integrated across different health services, maintaining confidentiality becomes more challenging but increasingly essential.
It is imperative that patients exert greater control over who has access to their records. This involves clear mechanisms for obtaining consent and allowing patients to understand how their data is used. EHRs should be able to provide patients with easy-to-use tools to grant or revoke access to their data, ensuring they remain in control. Only the necessary amount of patient information should be collected and shared to fulfill healthcare needs. EMRs should be designed to collect the minimum data required for healthcare purposes, thus reducing the potential for privacy breaches.
AI introduces complex challenges to maintaining data privacy and security, impacting both patients and healthcare providers. These challenges arise from the vast amounts of sensitive data AI systems need to function effectively, as well as the sophisticated nature of the technology itself. AI systems, especially in behavioral healthcare, will rely on large datasets to function accurately and provide meaningful insights. These datasets will invariably contain sensitive patient information, including medical histories, mental health and substance use records, and personal identifiers.
Behavioral healthcare systems and providers remain responsible for safeguarding patient data, and the sheer volume of information AI systems require increases their burden in ensuring all security measures, such as encryption and access controls, are in place and constantly updated. Providers must navigate complex consent management systems to ensure that they are not violating patient privacy, requiring robust tracking of consent permissions, which can be difficult to manage, particularly when dealing with highly sensitive behavioral health data that requires strict privacy controls under regulations like HIPAA and 42 CFR Part 2.
2. Technological Integration
Integrating new technologies with existing systems in behavioral healthcare presents a complex set of challenges. The process involves not only technical adjustments but also aligning with organizational workflows, regulatory compliance, and ensuring that the new technology adds value without disrupting existing services. The financial burden of implementing EHR systems remains a significant challenge, particularly for smaller BH organizations and providers. The high costs of purchasing, integrating, and maintaining these systems, along with training staff, can be prohibitive without external funding or governmental support.
Many BH organizations and providers operate with legacy systems that may be outdated but are critical for daily operations. Integrating modern technologies with these older systems can be difficult due to different software architectures, data formats, or communication protocols. Ensuring seamless data flow between new and existing systems is crucial and involves data mapping, format standardization, and developing interfaces that can handle the exchange of data accurately and efficiently.
New technologies should not only integrate with current systems but also be scalable and flexible enough to accommodate future upgrades and expansions without requiring complete overhauls. Integrating these new technologies involves changing existing processes and workflows, which can be met with resistance from staff accustomed to traditional methods. Effective change management strategies are essential to facilitate adoption, including training, support, and clear communication about the benefits of the new technology.
The rapid evolution of AI technology presents significant challenges for EHR systems, which must not only be capable of incorporating the latest AI innovations but also be flexible and adaptive enough to evolve alongside these advancements. In the context of AI-driven healthcare, the future of EHRs lies in their ability to support continuous innovation and integration of new AI tools and models. This means that an effective EHR system must go beyond static data management to become a dynamic platform that can seamlessly integrate and evolve with the latest AI functionalities. Traditional EHRs are often rigid systems designed primarily for data entry, storage, and retrieval but not for the seamless integration of cutting-edge AI technologies. To keep pace with AI advancements, EHRs must adopt modular architectures that allow for the rapid deployment of new AI models without requiring a complete overhaul of the system. For instance, if a new large language model (LLM) is developed that is significantly better at interpreting clinical notes or predicting patient outcomes, the EHR should be able to “swap in” this new model with minimal disruption to ongoing clinical workflows.
3. User Expectations
Patients are increasingly expecting their BH providers to offer the same level of technological accessibility and convenience that is now standard in many other areas of healthcare. The widespread adoption of EHRs and other digital tools in general medical settings has reset expectations, prompting patients to demand greater flexibility and transparency in their interactions with BH services. No longer satisfied with traditional methods of scheduling, communication, and care coordination, patients are increasingly looking for streamlined, tech-driven solutions that allow them to manage their healthcare with the same ease they manage other aspects of their lives.
One of the primary expectations from patients is the ability to schedule and cancel appointments without the hassle of making phone calls or leaving voicemails. Patients want to use digital platforms, such as apps or online portals, to manage their appointments at their convenience. This expectation aligns with the broader healthcare industry’s shift towards patient-centered care, where accessibility and convenience are prioritized. For BH providers, offering this capability not only enhances patient satisfaction but also reduces administrative burden, allowing front-office staff to focus on more complex tasks.
In addition to appointment management, patients are now expecting more involvement in their care plans. The ability to view lab results or progress notes through EHRs is no longer sufficient, and we expect patients to participate actively in their treatment process. Patients will need real-time access to their care plans, with the opportunity to provide feedback, set goals, and track their progress. This collaborative approach empowers patients, particularly those managing more chronic behavioral health conditions, to take a more proactive role in their wellness and recovery, leading to better engagement and outcomes.
Patients are looking for secure, asynchronous ways to communicate with their care teams. The demands of modern life often make it difficult to schedule time for in-person visits or phone calls. Instead, patients expect the ability to message their providers or care teams through secure portals or apps, where they can ask questions, request refills, or clarify aspects of their treatment plan at their convenience. This asynchronous communication can allow for more flexible interactions without disrupting the provider’s schedule, fostering a more responsive and accessible model of care.
As technology continues to transform healthcare, patients are increasingly expecting their BH providers to keep pace by offering user-friendly digital solutions. Behavioral health providers that adopt and implement these technologies will be better positioned to meet patient expectations, enhance engagement, and improve overall outcomes.
The future of EHRs isn’t just about keeping pace with technology—it’s about transforming the patient experience and creating a healthcare system that is more equitable and patient-centered. As advancements in AI, data analytics, and digital platforms continue to reshape the landscape, there’s an unprecedented opportunity to make EHRs not just more functional but more anticipatory of patient needs. Imagine a system where health records do more than store information—they guide care, predict health issues, and provide real-time insights that lead to better outcomes and more personalized care.
Now is the time for all stakeholders—patients, providers, and EHR companies—to step up and seize this moment of transformation. For patients, it’s about advocating for your own care, demanding the tools that allow you to engage fully with your wellness and recovery journey. Patients need to take advantage of existing patient portals, push for more user-friendly features, and embrace the technologies that allow them to take control of their wellness in real-time.
For BH providers, the shift to more accessible, AI-driven electronic health records means adapting to a new way of delivering care. It’s time to invest in systems that enhance communication, streamline workflows, and improve patient engagement. Embrace the potential of AI, use data-driven insights to guide clinical decisions, and collaborate with your patients to create care plans that are not only informed by their biopsychosocial history but enriched by real-time data. Patients expect a higher level of engagement, so meet them there with the tools that make it possible.
For EHR companies, the challenge is clear: innovation must be constant, and flexibility is key. As AI models improve and digital health platforms evolve, EHR systems must remain adaptable—able to incorporate new technologies, swap in superior models, and modify workflows in real-time. This is more than just a software upgrade; it’s a reimagining of how healthcare data should flow between providers and patients, how care should be delivered, and how health systems should function. Build systems that are not just ready for today but designed to evolve with tomorrow’s technologies.
The call to action is simple: let’s build a future where EHRs are a true catalyst for better behavioral healthcare—where patients are empowered, providers are supported, and innovation drives us all forward. Together, we can harness the full potential of accessible EHRs and technology to create a more responsive, efficient, and patient-centered behavioral system of care and wellness.